When it comes to cognitive decline in older adults, it’s important to understand the difference between Alzheimer’s and dementia. Although the terms are often used interchangeably, they are not the same condition. Alzheimer’s is a specific type of dementia that accounts for 60-80% of cases. Dementia, on the other hand, is an umbrella term for a range of cognitive impairments that interfere with daily life.
One key distinction between Alzheimer’s and dementia is that Alzheimer’s is a progressive brain disease that leads to memory loss and cognitive decline. On the other hand, dementia is a syndrome that can be caused by various conditions, including Alzheimer’s. It’s crucial for caregivers and healthcare professionals to recognize the nuances between the two in order to provide appropriate care and support for individuals affected by these conditions.
Symptoms and Progression Variances
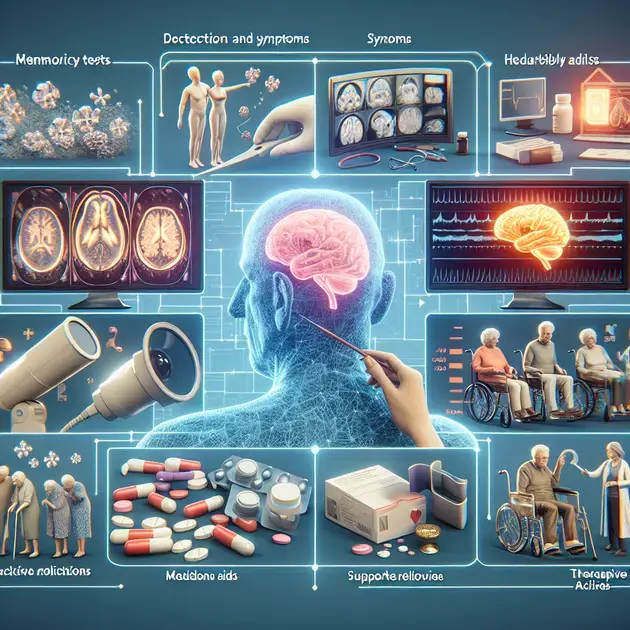
When it comes to understanding the difference between Alzheimer’s and Dementia, it is crucial to recognize the symptoms and progression variances that differentiate the two conditions. Alzheimer’s disease typically starts with memory loss, while Dementia encompasses a range of cognitive impairments. To identify the specific symptoms of each condition, individuals can use online resources such as the Alzheimer’s Association website, which provides detailed information on the signs and progression of both illnesses.
Monitoring the gradual decline in cognitive functions, such as memory, reasoning, and language skills, can help differentiate between Alzheimer’s and Dementia. Apps like “MindMate” offer tools for tracking cognitive changes and provide insights into the varying symptoms associated with each condition. By recording and analyzing these differences over time, individuals and caregivers can better understand the unique progression variances of Alzheimer’s and Dementia.
Step-by-Step Guide:
1. Visit the Alzheimer’s Association website or download their app for comprehensive information on Alzheimer’s and Dementia symptoms.
2. Use “MindMate” app to monitor and track cognitive functions to identify specific progression differences between the two conditions.
3. Consult with healthcare professionals for a detailed evaluation and diagnosis based on observed symptoms.
Diagnosis and Treatment Approaches
Diagnosing and treating Alzheimer’s and Dementia require distinct approaches due to the differences in their underlying causes and progression. Medical websites like Mayo Clinic offer detailed insights into the diagnostic procedures and treatment options available for both conditions. Understanding the diagnostic criteria and treatment approaches is essential for effectively managing the symptoms and slowing down the progression of Alzheimer’s and Dementia.
Medical professionals utilize a combination of cognitive assessments, brain imaging scans, and blood tests to diagnose Alzheimer’s disease accurately. In contrast, Dementia diagnosis involves evaluating various cognitive functions and identifying potential reversible causes. Apps such as “CogniFit” provide cognitive assessments that can aid in the early detection and diagnosis of Alzheimer’s and Dementia through online cognitive tests.
Step-by-Step Guide:
1. Visit the Mayo Clinic website to learn about the diagnostic procedures and treatment options for Alzheimer’s and Dementia.
2. Use the “CogniFit” app to conduct cognitive assessments and detect early signs of cognitive decline associated with both conditions.
3. Consult with healthcare providers to explore personalized treatment approaches based on the specific diagnosis of Alzheimer’s or Dementia.
Impact on Daily Living and Support Strategies
The impact of Alzheimer’s and Dementia on daily living can be significant, affecting various aspects of an individual’s life and requiring tailored support strategies. Reliable sources like the Alzheimer’s Society offer guidance on how to manage daily challenges and provide support for individuals living with these conditions. Understanding the impact on daily activities like personal care, communication, and social interactions is crucial for developing effective support strategies.
Apps such as “Alzheimer’s Caregiver Buddy” are designed to assist caregivers in managing daily tasks and creating supportive environments for individuals with Alzheimer’s or Dementia. These resources offer practical tips, schedules, and communication tools to enhance caregiving and promote the well-being of both patients and caregivers.
Step-by-Step Guide:
1. Refer to the Alzheimer’s Society website for insights into the impact of Alzheimer’s and Dementia on daily living and effective support strategies.
2. Download the “Alzheimer’s Caregiver Buddy” app to access tools and resources for managing daily tasks and providing quality care for individuals with these conditions.
3. Engage in support groups and counseling sessions to gain emotional support and practical advice on coping with the challenges of Alzheimer’s and Dementia.
**Symptoms and Progression Variances**
Diagnosis and Treatment Approaches
When it comes to identifying and addressing symptoms and progression variances in individuals, a thorough diagnostic process is essential. Medical professionals utilize a range of tools and assessments to determine the underlying cause of the symptoms being experienced. This may involve physical examinations, imaging tests, blood work, and cognitive evaluations. By pinpointing the specific factors contributing to the variances in symptoms and progression, healthcare providers can create targeted treatment plans.
In terms of treatment approaches, the methods employed can vary based on the individual’s unique needs and the underlying condition causing the symptoms. For individuals experiencing symptoms and progression variances related to neurological conditions, such as multiple sclerosis or Parkinson’s disease, treatment may involve a combination of medication, physical therapy, and lifestyle modifications. It is crucial for healthcare providers to regularly monitor the individual’s response to treatment and make adjustments as needed to optimize outcomes.
Furthermore, early diagnosis and intervention play a significant role in managing symptoms and progression variances effectively. By promptly identifying the underlying cause and implementing appropriate treatment approaches, healthcare providers can help individuals better manage their condition and potentially slow the progression of symptoms. This highlights the importance of routine screenings and proactive healthcare measures in addressing symptoms and progression variances.
Collaboration between healthcare professionals, individuals, and their support networks is also vital in navigating the complexities of symptoms and progression variances. By fostering open communication and shared decision-making, all stakeholders can work together to develop comprehensive treatment plans that prioritize the individual’s well-being and quality of life.
Impact on Daily Living and Support Strategies
The impact of symptoms and progression variances on daily living can be profound, affecting various aspects of an individual’s life. From challenges with mobility and communication to cognitive impairment and emotional well-being, these variances can significantly impact the individual’s ability to perform daily tasks and engage in social interactions.
Developing effective support strategies is crucial in helping individuals navigate the challenges posed by symptoms and progression variances. This may involve creating a supportive environment that promotes independence and safety, as well as providing access to resources and services that cater to the individual’s specific needs. Support networks comprising family members, friends, healthcare providers, and community organizations can play a pivotal role in offering emotional support, practical assistance, and guidance throughout the individual’s journey.
Implementing adaptive strategies and assistive technologies can also enhance the individual’s ability to cope with symptoms and progression variances. From mobility aids and communication devices to personalized care plans and behavioral interventions, these tools can empower individuals to maintain their autonomy and quality of life despite the challenges they may face.
Educating individuals and their support networks about symptoms and progression variances is essential in fostering a collaborative approach to care. By increasing awareness and understanding of the condition and its impact, stakeholders can work together to develop effective coping mechanisms, problem-solving skills, and resilience in the face of adversity.
conclusão
In conclusion, the diagnosis and treatment of symptoms and progression variances require a comprehensive approach that involves thorough diagnostic processes and targeted treatment plans tailored to individual needs. Early intervention and collaborative efforts among healthcare professionals, individuals, and support networks are crucial in effectively managing the impact of these variances on daily living.
By prioritizing proactive healthcare measures, regular screenings, and open communication, stakeholders can work together to develop comprehensive treatment plans that focus on the well-being and quality of life of those experiencing symptoms and progression variances. Utilizing a combination of medication, therapy, and lifestyle modifications can help individuals better cope with neurological conditions and potentially slow the progression of symptoms.
Support strategies play a pivotal role in assisting individuals in navigating the challenges posed by symptoms and progression variances. From creating supportive environments to implementing adaptive technologies, these interventions empower individuals to maintain autonomy and quality of life despite the hurdles they face. By educating individuals and support networks about these variances, stakeholders can foster resilience, problem-solving skills, and effective coping mechanisms in the face of adversity.